Childhood Cancer Survivors
Kidneys
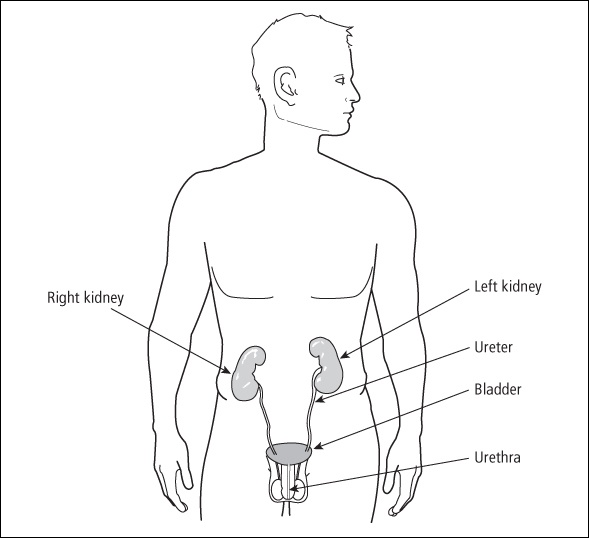
The kidneys, the main organs of the excretory system, are located at the bottom of the ribcage near the back of the body. These two bean-shaped organs are each about the size of a fist.
Blood enters the kidneys from branches off the aorta (the main blood vessel that carries oxygen-rich blood from the heart). The kidneys regulate blood pressure, filter waste products from the blood, and control the amount of water, minerals, and vitamins in the blood that returns to the body. Inside each kidney are millions of microscopic structures that filter out large particles, such as white and red blood cells and most proteins, allowing them to return to the bloodstream. What remains in the kidney after this process is the yellow liquid called urine. Urine flows from the kidneys through long tubes (ureters) into the bladder, where it is stored until it is eliminated from the body by urination. Figure 14-1 shows the location of kidneys and bladder within the body.
Organ damage
The kidneys can be impacted by surgery, chemotherapy, and radiation. The majority of children with Wilms tumor have one kidney removed. If they only receive a short cycle of chemotherapy and no radiation, the remaining kidney usually functions with no major problems. The remaining kidney enlarges and does the work of two kidneys. Protecting the remaining kidney is discussed later in this chapter, under “Medical management.”
The vast majority of survivors of childhood cancer have good kidney function. The few long-term effects that do develop are rare. These include nephritis, high blood pressure, renal artery damage, and tubular necrosis.
Radiation
Radiation delivered directly to the kidneys can cause dysfunction. Survivors who are at highest risk include those who received:
-
Radiation to the whole abdomen for soft tissue sarcomas of the pelvis or abdomen; tumors of the kidney, abdomen, or pelvis; or abdominal lymphomas.
-
Total body radiation (TBI) before undergoing stem cell transplantation (e.g., bone marrow transplant, peripheral stem cell transplant, or cord blood transplant).
Chronic nephritis (inflammation of the kidneys) can develop after 2000 centigray (cGy) or more of radiation to an entire kidney. If chemotherapy is given as well, lower doses of radiation (1000 to 1500 cGy) can cause injury. Chronic nephritis is also seen in stem cell transplant survivors who had TBI as part of their conditioning regimen. The likelihood of nephritis developing appears to depend on which chemotherapy drugs the survivor had prior to the transplant.
Chronic nephritis can develop during treatment or years after treatment is completed. It can lead to kidney failure or heart damage and thus requires close medical surveillance. Improved radiation techniques and kidney shielding have decreased the number of cancer survivors who develop nephritis.
The kidneys also help regulate blood pressure. High blood pressure (hypertension) means the heart is working overtime to push blood through arteries. High blood pressure can lead to heart disease, hardening of the arteries (atherosclerosis), or stroke.
Lisa had high-dose Cytoxan ® and six doses of total body irradiation prior to getting her bone marrow transplant. A year later her hemoglobin and platelets started to drop. It took months to figure out that it was kidney damage. The kidney doctor said that if the radiation damages the kidneys, it usually shows up between 6 months and a year post-transplant. Her kidney filtration rate was only 40 percent. She’d retain fluid in her feet and she developed high blood pressure. Her potassium also got high. Just when we thought things were fine, boom, we got hit with this.
She started out taking four bicarbonate pills a day, medication for her high blood pressure, and weekly injections. One of the jobs the kidneys do other than filter is to produce a chemical that tells the bone marrow to make red blood cells. Her marrow was full of precursor cells, but they weren’t developing into red cells. When the kidney damage is great enough, not enough of this chemical is released, so a drop in hemoglobin occurs. So she began getting Epogen ® (a drug used to treat anemia) injections on a weekly basis. It takes about 6 weeks to see the hemoglobin go back up, and it took weeks to figure out the exact dosage required to maintain her hemoglobin level. I assumed the damage was permanent and the injections would be a lifelong thing.
Suddenly, about a year later, we noticed her hemoglobin was too high and we started inching down her injections. Then we stopped the injections and waited to see what happened. Her hemoglobin levels continue to inch up at a really slow rate. She also had high creatinine and BUN (blood urea nitrogen) levels, and electrolyte imbalances, but all that seems okay for the moment.
Another rare late effect in long-term survivors who were treated with radiation to a field that included one or both kidneys (this includes Hodgkin lymphoma survivors who had their spleens irradiated) is renal artery damage or blockage. The main symptom is very high blood pressure that occurs years after treatment.
Chemotherapy
High doses of cisplatin can affect the kidneys. Some children or teens who received cumulative doses of more than 450 mg/m 2 of cisplatin can develop acute renal toxicity during treatment. 1 Over time, a kidney can sometimes repair itself. In other cases, survivors need to take replacement magnesium. Cisplatin damage usually becomes apparent during or within a year after treatment. Carboplatin is less toxic to the kidneys; however, in combination with other therapies, it can also impact renal function.
Jamie had acute renal failure on treatment, which resolved without dialysis, thank goodness. After the catheter was removed, Jamie suffered horribly for 2 weeks with kidney stones. His lab reports showed extremely high levels of uric acid and creatinine in his urine. This has since normalized. His first glomerular filtration rate (GFR) showed his kidneys functioning at 52 percent. Two months later, function was at 75 percent, and in the next 2 months it was at 95 percent. A huge improvement.
High doses of cyclophosphamide and/or ifosfamide can cause necrosis (death) of tubules in the kidneys. If these drugs are given with radiation to the pelvis or abdomen, or if combined with other drugs that can damage the kidneys, the risk of kidney problems increases. These changes usually occur only in survivors who have had multiple relapses and received extremely high doses of these drugs.
My daughter was treated for rhabdomyosarcoma. One of the chemotherapy agents she received was ifosfamide, which caused renal tubular acidosis. The oncologist told me the ifosfamide affected her kidneys’ ability to process electrolytes. Her serum bicarbonate level was low, so her body’s pH was low. With a low pH, you don’t grow. She takes two supplements, Bicitra ® and Neutraphos ® , which keep her levels on the high side. This has met with some success. Though she still has a long way to go to catch up, she is now growing at a normal rate.
Some chemotherapy drugs, when combined with radiation, can increase the risk of late effects to the kidneys. 2 These drugs include the following:
-
Ifosfamide
-
Cytoxan
-
Cisplatin
-
Carboplatin
-
Dactinomycin
Persistent problems usually only develop in survivors who had severe kidney problems during treatment.
My daughter was born with neuroblastoma. Her first two pea-sized tumors and her adrenal gland were removed when she was 1 month old, but she relapsed 3 months later. The new tumor was treated with Cytoxan ® (cyclophosphamide), VP-16, cisplatin, Adriamycin ® , ifosfamide, and vincristine in different combinations for over a year. Although the tumor stopped growing on chemo, it could not be surgically removed. It sat right on top of her left kidney and flattened it out. The tumor partially blocked the ureter and she started getting bladder infections. We monitored her kidney closely, and it failed after 5 months. She had a nephrostomy tube placed in 1993 and surgery a few months later to reroute her ureter around the tumor. She has had no problem with her bladder or kidneys since. She’s now 8 years old.
Signs and symptoms
Signs and symptoms of kidney damage include the following:
-
Fatigue
-
Anemia
-
Excessive urination during the night (nocturia)
-
Weakness
-
Retaining fluid (edema)
-
High blood pressure
-
Poor growth (this can be a sign of very poor kidney function)
Screening and detection
Survivors who received chemotherapy that can cause kidney problems need an evaluation of kidney function after the end of treatment. Survivors who were treated with chemotherapy and radiation to the abdomen or a kidney need an evaluation of kidney function either annually or every other year. Your evaluation should include the following:
-
Physical exam
-
Health history, including questions about frequency of urination, painful urination, and bedwetting
-
Blood pressure
-
Urinalysis
-
Blood tests for BUN and creatinine levels
For a complete list of the tests you should have based on your treatment, you and your healthcare provider can refer to the Children’s Oncology Group’s survivorship guidelines at www.survivorshipguidelines.org .
Medical management
If you have long-term kidney toxicities from treatment, you should be seen by a pediatric or adult nephrologist (kidney specialist). Because damage to the kidneys can resolve over time, expert medical care is needed while waiting to see if recovery occurs. In the very rare cases in which progressive kidney failure occurs, dialysis and/or kidney transplant may be necessary.
If you had radiation to one or both kidneys, regular checks of your blood pressure should be part of your medical care. You should visit your healthcare provider’s office or your school clinic several times a year to have your blood pressure checked. Steps you can take to help keep your blood pressure in the healthy range are maintaining a normal weight, exercising daily, and eating less salt.
The primary concern of survivors with only one kidney (after treatment for Wilms and occasionally neuroblastoma) is protection of the remaining kidney. The kidney is naturally very well protected within the body. However, you should talk with your healthcare provider about the sports you play. Your healthcare provider may recommend that you avoid contact sports or use a kidney guard if you do participate. Each family needs to balance quality of life issues with protection when making decisions about sports activities.
My son Danny had Wilms when he was an infant and they took out half his kidney. He’s now 10 and is a sports fanatic. He plays football, and I got him an abdominal protector that clips to the bottom of his shoulder pads. It is a hard shell with padding inside. It goes all the way around his abdominal area and hooks in the front. When Danny started wearing it the other boys all wanted one too. Instead of being the oddball, he began a new fad. I call him “the kid in armor.”
Survivors with one kidney should also know the signs of urinary tract and kidney infections and seek treatment quickly to protect their single kidney. If you have burning upon urination, blood in the urine, painful urination, an urgent need to urinate frequently, or flank pain on the side of the remaining kidney, go to your healthcare provider as soon as symptoms develop.
There are certain categories of drugs, including some types of antibiotics, that can affect renal function. If you only have one kidney, don’t use over-the-counter, herbal, or other medications without first discussing them with your nephrologist. Many of these are toxic to the kidneys, including non-steroidal anti-inflammatory drugs (e.g., aspirin, ibuprofen, and naproxen) for pain, fever, or inflammation. Remind your healthcare provider anytime she gives you a prescription that you have only one kidney.
Survivors with only one kidney need to make sure their healthcare providers know of their special circumstances. Putting a card in with your driver’s license that says you have only one kidney and/or wearing a medical alert bracelet will assist you in the unlikely event that you need medical care and are unable to tell emergency responders that you have a single kidney.
Table of Contents
All Guides- 1. Survivorship
- 2. Emotions
- 3. Relationships
- 4. Navigating the System
- 5. Staying Healthy
- 6. Diseases
- 7. Fatigue
- 8. Brain and Nerves
- 9. Hormone-Producing Glands
- 10. Eyes and Ears
- 11. Head and Neck
- 12. Heart and Blood Vessels
- 13. Lungs
- 14. Kidneys, Bladder, and Genitals
- 15. Liver, Stomach, and Intestines
- 16. Immune System
- 17. Muscles and Bones
- 18. Skin, Breasts, and Hair
- 19. Second Cancers
- 20. Homage
- Appendix A. Survivor Sketches
- Appendix B. Resources
- Appendix C. References
- Appendix D. About the Authors
- Appendix E. Childhood Cancer Guides (TM)