Newborn Screening for Early Childhood Cancer Predisposition Syndromes
Funded 2025

Collaborators:
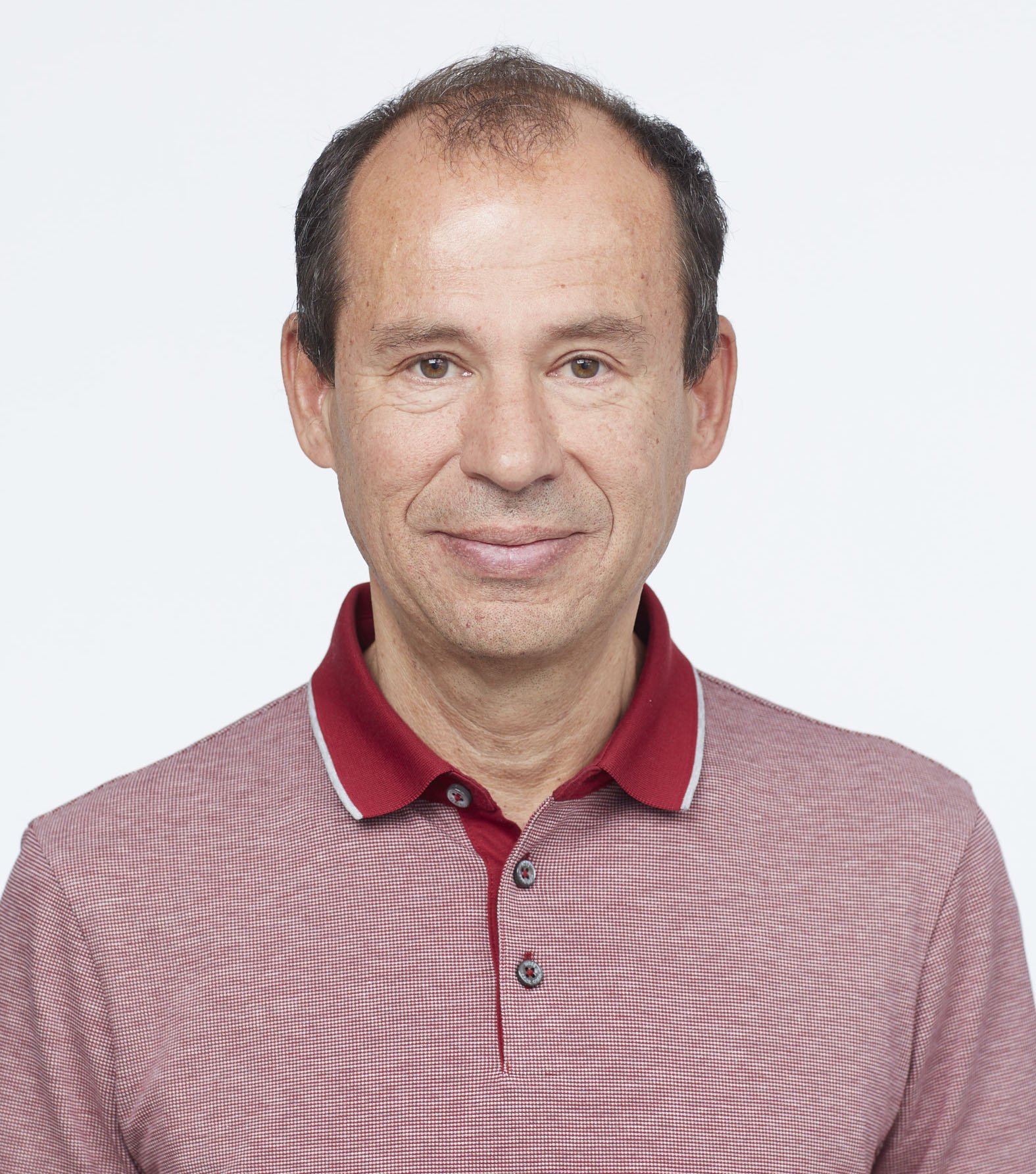
- Team Leader: Sharon Plon, MD/PhD, FACMG, Baylor College of Medicine
- Donald W. (Will) Parsons, MD/PhD, Baylor College of Medicine
- Lisa Diller, MD, Dana-Farber Cancer Institute
- Philip Lupo, PhD, Emory University
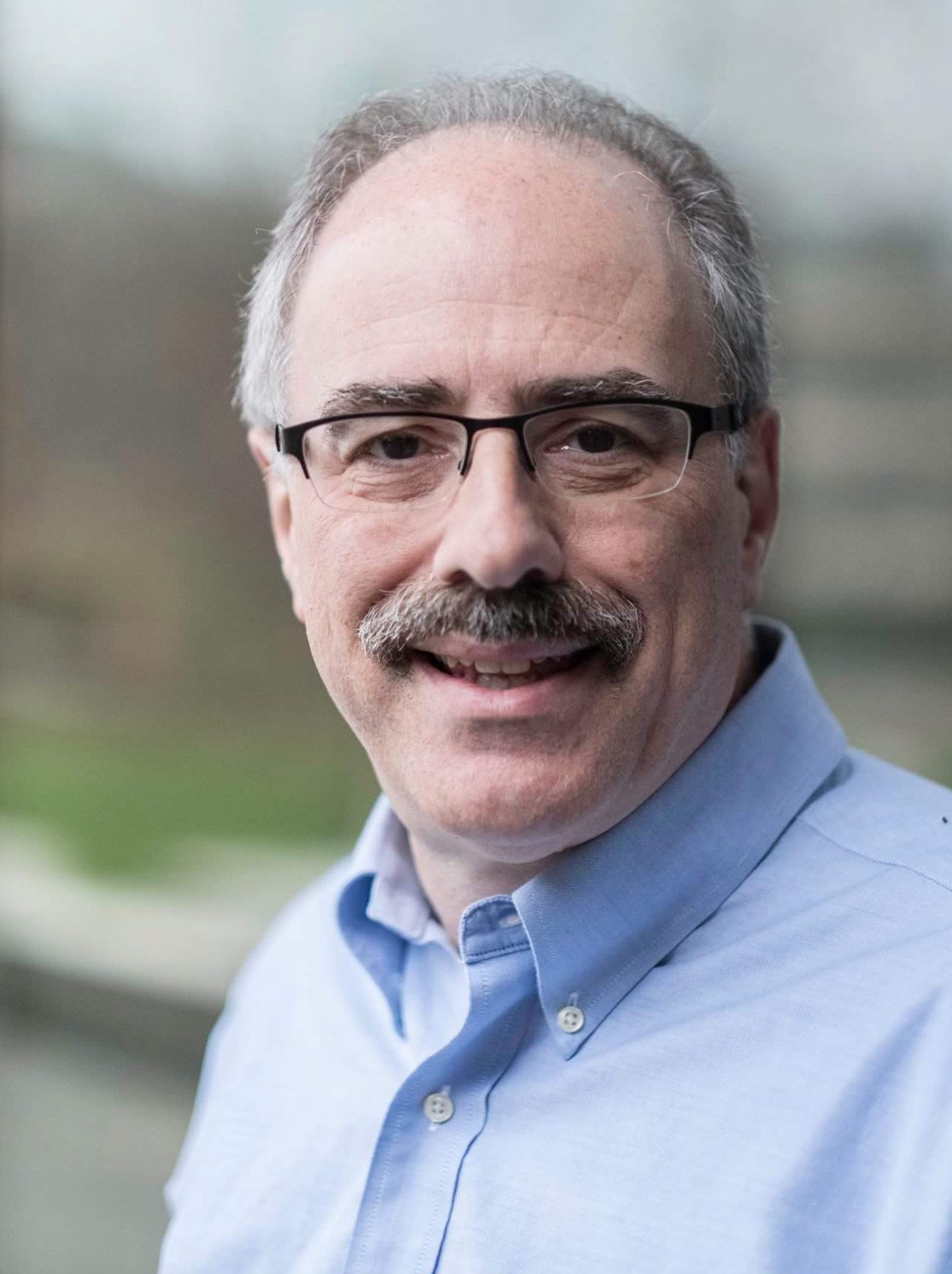
- Richard Parad, MD, Brigham and Women's Hospital
- Stacey Pereira, PhD, Baylor College of Medicine
- Sarah Scollon, MS, CGC, Baylor College of Medicine
The Goal: To make newborn screening for cancer risk genes a reality.
Every newborn in the United States gets a “heel-stick” blood test to check for certain rare diseases, but cancer risk isn’t included.
Led by co-principal investigators Dr. Sharon Plon and Dr. Lisa Diller, this Crazy 8 team will study the implementation and promise of a genetic test using this newborn blood samples, to screen for several cancer predisposition syndromes. The team has identified nine genes that could signal a high risk for early-onset cancers, including the RB1 gene which can cause retinoblastoma, a type of eye cancer. If identified early, babies with a faulty RB1 gene could receive eye exams and treatment before the cancer progresses preserving their eyesight and their lives.
The team’s goal is to develop an affordable, AI-supported genetic test to screen newborn blood samples. They will also create educational materials for parents and test them in Boston and Houston to see how parents and pediatricians respond to this new screening. If successful, the research will help push for nationwide adoption of newborn cancer risk screening.
Read more