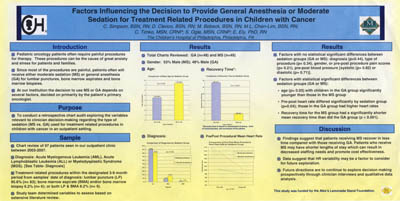
Factors Influencing the Decision to Provide General Anesthesia or Moderate Sedation for Treatment Related Procedures in Children with Cancer
Update:
Catherine Timko, MSN, CRNP and Danielle Clerico, BSN, RN presented a research talk, “A Mixed Method Approach to Analyzing Clinician Decision Making for Procedural Sedation in Children with Cancer” at the Association of Pediatric Hematology and Oncology Nurses (APHON) 34th Annual Conference; October 2010.
This presentation was also an invited presentation at the Children’s Hospital of Philadelphia annual Nursing Research and Evidence Based Practice Grand Rounds in December 2010.
The purpose of this research is to explore and delineate the variables relevant to clinician (Nurse Practitioner [NP] & Physician [MD]) and family decision-making about the type of sedation (moderate sedation [MS] vs general anesthesia [GA]) used for cancer treatment related procedures (e.g. lumbar puncture [LP], bone marrow aspirate [BMA]) in children with cancer. We propose over a two year period of time to address the following specific aims.
-
Aim 1 (Year 1) Using a retrospective chart audit we will identify the patient/family, clinician, and disease related characteristics that influence decision making in determining if a child undergoing treatment for cancer receives MS or GA for diagnostic procedures. Aim 1b We will also compare and contrast the variables identified from chart review between the 2 different groups (MS & GA).
- Aim 2 (Year 2) We will explore clinician decision making related to sedation choice (MS vs GA) for children with cancer undergoing diagnostic procedure through qualitative, scripted interviews.
Poster Presentation:
Association of Pediatric Hematology/Oncology Nurses (APHON) Conference Poster, Orlando, FL, September 2009: