By: Trish Adkins
Nearly 5,000 children will be diagnosed with a brain tumor in the United States this year. For those children, the prognosis and treatments will vary, but one thing is certain: their regular childhoods will be interrupted as they fight for a cure. That fight will include hospital stays and missed days of school. It will also include something else: hope.
Because while pediatric brain tumors happen, so does research.
Here are the facts you need to know about pediatric brain tumors and how you can help kids:
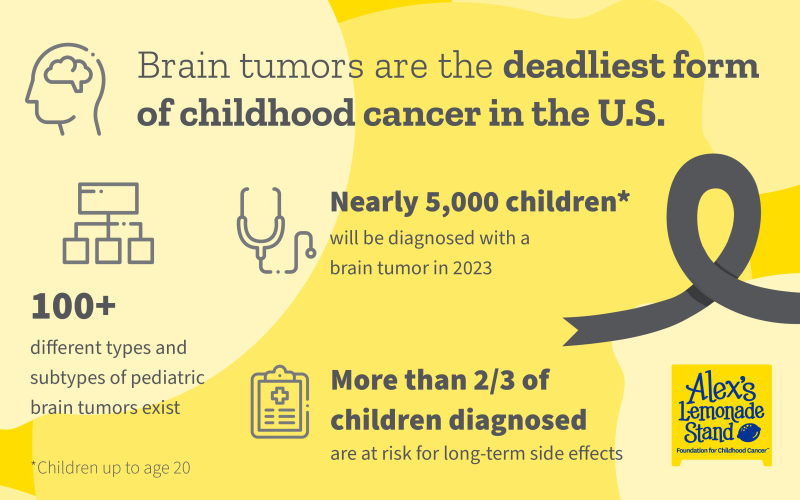
1. Brain tumors are the deadliest form of childhood cancer in the United States, accounting for a third of all pediatric cancer deaths each year.
In 2016, brain tumors earned this top spot as a result of the decline in pediatric leukemia death rates. Research, breakthroughs and changes to the standard of care led to the incredible leukemia success story and the same can happen for brain tumors. Through its comprehensive research grant program, Alex’s Lemonade Stand Foundation (ALSF) funds research grants that study the mechanisms of brain tumors and test potential drugs in clinical trials. 
2. The overall five-year survival rate is around 75% for children diagnosed with brain tumors. But some tumors like DIPG, a type of high-grade glioma, have a 0% five-year survival rate.
The disparity in survival rates across tumor types is because each type of pediatric brain tumor is different. There is no one-size-fits-all treatment that works equally well for a high-grade glioma and for a medulloblastoma. This is what makes varied research such a critical step towards cures for all children.
3. Over 60% of childhood brain tumors are found in the posterior fossa of the brain — the area that houses some of the most critical structures of the brain.
The posterior fossa, found in the back of the brain, is home to the cerebellum, which controls balance and motor skills, and the brain stem, which controls the critical functions of the body such as blood pressure and breathing.
4. According to the World Health Organization (WHO), there are more than 100 types and subtypes of primary brain tumors, each differentiated by where they occur, the kind of cells they are made of, and what genetic mutations they contain.
Ten years ago, brain tumors were classified by two criteria: their appearance under the microscope and their location in the central nervous system. Now, tumors can be further defined based on their genetic features which can help to guide doctors toward precision treatments.
The most common tumors include medulloblastoma, juvenile pilocytic astrocytoma (JPA), ependymoma, diffuse intrinsic pontine glioma (DIPG) and atypical teratoid rhabdoid tumor (AT/RT).
5. Brain tumor survivors are at risk for a bevy of long-term side effects that can affect every aspect of their life.
Two-thirds of all children diagnosed with cancer are at risk for long-term side effects caused by both the tumor and the treatment. Side effects can include cardiac dysfunction, secondary cancers, memory loss, motor skill dysfunction, impaired balance, decreased muscle tone and hearing loss. These long-term side effects can have impacts on school, work, and quality of life.
6. When the standards of care — surgery, radiation and chemotherapy — fail, children who are facing relapsed disease need options.
Clinical trials represent the best hope for children with refractory or relapsed disease. Trials study the safety and effectiveness of new therapies that have shown success in the lab or with other diseases, with the goal of providing new standards of care.
7. You can help be part of the solution by supporting research.
Each of us can make a difference for children battling brain tumors by spreading awareness and working to fund groundbreaking research happening right now. Scientists like ALSF-funded researcher, Dr. Nada Jabado, are working to match genetic targets in tumors to drugs with cures in mind.
“What I can’t treat today, I will be able to treat, tomorrow,” said Dr. Jabado.
Support Pediatric Brain Tumor Research.
Sources: CDC, CBTRUS, WHO
Updated May 1, 2024
First Published:

