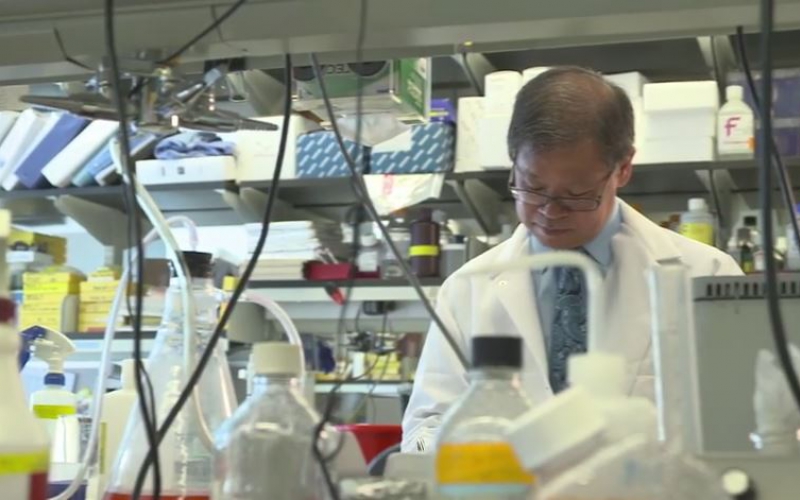
ALSF Innovation grantee Darrell Yamashiro works in the lab at Columbia University Medical Center. Dr. Yamashiro works with Dr. Julia Bender-Glade (mentioned below) developing therapies for relapsed childhood cancer.
by Trish Adkins
Gone are the days of just chemotherapy and radiation. Today’s researchers and oncologists are combining the traditional tools with cutting-edge biological medicine, genetic analysis and novel therapeutics in the labs and clinics.
Childhood cancer researchers are working hard towards better treatments and more cures every single day. Here are five trends in research today:
1. Treating the patient, not just the cancer
For over 40 years, scientists have known about oncogenes, the abnormal genes that can drive the growth of abnormal cells that become cancer. Now, childhood cancer researchers are discovering more about oncogenes and finding new ways to stop the development of cancer by targeting these “bad” genes. Researchers are also studying the biology of children with cancer to determine the best way to treat cancer within their body.
“Every cancer is different, because every child is different,” said Dr. Julia Glade-Bender, a member of the ALSF Scientific Advisory Board and an oncologist at New York-Presbyterian Hospital/Morgan Stanley Children’s Hospital. Dr. Glade-Bender directs the Developmental Therapeutics Program at NYP, which works to identify the molecular drivers of each child’s cancer. Researchers will then use that information to personalize treatment using novel, biologically targeted agents during clinical trials.
2. CAR T cell immunotherapy
In August 2017, the FDA approved CAR (Chimeric Antigen Receptor) T cell immunotherapy as a treatment for certain types of acute lymphoblastic leukemia (ALL). This is the first gene therapy to achieve FDA approval in the United States and one of the few major breakthroughs and approvals for pediatric oncology in recent years.
Like other types of immunotherapy, CAR T cell therapy harnesses a patient’s immune system to fight and destroy cancer cells. The FDA approval does not just bring hope for children battling relapsed ALL; it opens the door for more innovative research for all types of childhood cancer.
“The anticipation is that this is the first step towards changing the landscape of how we treat pediatric leukemia. The vision is that ultimately, we can remove a lot of the standard chemotherapy that we use and replace it with CAR T cell therapy. It’s not something that is going to happen overnight, but I truly believe it is where we will end up,” said Dr. Rebecca Gardner, a physician at Fred Hutchinson Cancer Research Center and ALSF Young Investigator Grantee.
Dr. Gardner recently led a clinical trial using CAR T cell therapy as a treatment for relapsed leukemia. In her trial, 93% of patients reached remission, after struggling to reach remission using traditional leukemia treatments.
3. Big data for big cures
Collaboration in the pediatric oncology research community has driven science closer to cures; however, with millions of disconnected data points, critical information is often filed and forgotten.
The Childhood Cancer Data Lab, powered by ALSF, is building a data refinery. This is a central location to collect, harmonize, analyze and share childhood cancer data. The data refinery will provide access to the entire field of pediatric oncology.
Researchers will quickly connect their findings to the findings of other colleagues from around the world. This allows them to identify common patterns and apply these hidden connections toward the development of new therapies to accelerate cures for children.
The data refinery is set to launch in beta in March 2018.
4. Engineering cures
ALSF Young Investigator Grantee, Dr. Steven Jonas from UCLA is developing tools to make the delivery of treatments like CAR T cell immunotherapy, quicker and more cost-effective.
His research project focuses on developing and applying microfluidics—the technology that makes things like ink-jet printers work—to speed up the process of altering individual children’s T cells into the immunotherapy drugs that could ultimately cure their cancer.
Researchers are also using nanotechnology to support immunotherapy treatments. Dr. Christopher Jewel, ALSF ‘A’ Award Grantee from the University of Maryland, studied the use of nanoparticles—small biodegradable particles—in conjunction with an experimental cancer vaccine for neuroblastoma. The nanoparticles are loaded with signals that stimulate the body’s immune system to fight cancer.
5. Harnessing viruses to kill cancer
Researchers have long known that cancer cells are hiding from the body’s immune system. In addition to uncovering these cells through immunotherapy, researchers are also using viruses to infect cancer cells and trick the immune system into killing cancer cells. Called oncolytic virotherapy, this cutting-edge research uses altered versions of viruses like HIV, polio and herpes to fight leukemia, brain tumors and other solid cell tumors.
ALSF Reach Grantees, Drs. Michael Burke and Jeffrey Medin, from the Children’s Hospital of Wisconsin, are using a virus to treat acute myeloid leukemia (AML). Drs. Burke and Medin take a small number of leukemia cells from a patient and infect those cells with a virus outside of the body. The virus then tricks leukemia cells into making a protein called interleukin 12 (IL-12). When IL-12 cells are returned to the patient’s body, their immune system sees the infected cells and begins attacking the leukemia cells.
The ALSF Grants Program is designed to fill critical voids in pediatric cancer research. ALSF works to fund all phases of research through 13 different grant programs. Each potential project is given careful consideration and reviewed by a team of leading scientists and clinicians. The result: ALSF is able to power breakthroughs and move closer to cures for childhood cancer. Learn more about the ALSF grants program here.

